Modernization of Cosmetics Regulation Act-MoCRA FDA Modernization of Cosmetics Regulation Act of 2022 – MoCRA The Modernization of Cosmetics Regulation Act of 2022 (MoCRA) has finally been signed into law by the U.S. Food and Drug Administration (FDA). This legislation will bring much-needed regulatory oversight to the cosmetic industry, ensuring the safety and well-being of consumers. Companies will now be held accountable for providing the safety and effectiveness of cosmetic products as positive changes toward consumer safety are anticipated. MoCRA is intended to harmonize the FDA’s regulatory power over cosmetics with other sectors such as drugs, medical devices, and foods. This goal is primarily achieved by mandating cosmetic manufacturers to register their facilities and list their cosmetic products with the FDA, ensuring better monitoring of these facilities and cosmetic products. Furthermore, the FDA intensifies its scrutiny of cosmetic safety through requirements like adverse event reporting, GMP adherence, recordkeeping, and proper cosmetic labeling. Key Components of MoCRA: 1-Facility Registration & Product Listing: All domestic and foreign manufacturers and processors are required to register their facilities with the FDA and must renew this registration biennially. Existing cosmetic facilities must comply with this rule by December 29, 2023, and new facilities must do so within 60 days of commencing operations. A responsible party must list each cosmetic product marketed in the U.S. with the FDA, including the product’s ingredients, manufacturer facility location, and product label, and update this information annually. Cosmetic products introduced to the market after December 29, 2023, must be listed within 120 days of commercial distribution at the latest. 2-Cosmetic Safety Substantiation Companies and individuals engaged in the production and distribution of cosmetics are responsible for substantiating their products’ safety. Neither the MoCRA nor FDA regulations mandate any specific tests or standards to establish individual products’ safety or their constituent ingredients. According to MoCRA, ‘adequate substantiation’ is tests, studies, analyses, research, or any other evidence deemed acceptable by knowledgeable scientific experts. A responsible party must establish records demonstrating sufficient safety substantiation for their cosmetic products. Manufacturers can utilize pertinent safety data to validate the safety of their products. Animal testing is not mandatory for the marketing of a cosmetic product. 3-Adverse Events, Recordkeeping and Reporting: Manufacturers must maintain records of health-related adverse events for 6 years (the number would be only 3 years for small businesses). These records must be available to the FDA and can be requested at any point. A responsible party must report serious adverse events to the FDA within 15 business days following the receipt of the report, along with a copy of the cosmetic retail packaging label. The definition of ‘serious adverse event,’ according to MoCRA, includes events resulting in significant disfigurement or alteration of appearance. 4-GMP & Labeling: Cosmetic facilities must follow Good Manufacturing Practices- GMPs aligned with national and international standards to ensure cosmetic product safety. The FDA can inspect facilities and access necessary records for GMP compliance. Manufacturers must demonstrate compliance with U.S. safety standards through adequate testing and substantiation, defined as scientific evidence. MoCRA instructs the FDA to release enforceable regulations regarding Good Manufacturing Practices (GMP) for cosmetic manufacturers by December 29, 2025 According to MoCRA, cosmetic product labels must have domestic or electronic contact info where the adverse events can be submitted. Cosmetics must list fragrance allergens to inform consumers. The MoCRA additionally requires a statement for use by industry professionals. 5-MoCRA Exemptions: Small businesses whose average gross annual U.S. sales for the past three years is below 1,000,000 USD are exempt from some MoCRA requirements such as GMP, facility registration, and product listing (optional registration will still be available for such small businesses). Certain cosmetic products are not eligible for the exemption, such as items that frequently have contact with the eyes or cosmetics for internal use, injectables, and long-lasting cosmetics, and must comply with MoCRA regardless of sales numbers. 6-FDA Enforcement: MoCRA holds authority above all state and local laws pertaining to cosmetic product safety. The FDA can access and copy certain records if a product poses a health threat and can order a recall if a cosmetic poses health risks and the responsible person refuses a voluntary recall. The FDA also has the authority to suspend a facility’s registration if it determines that a cosmetic product produced or processed by that registered facility and distributed in the United States carries a reasonable risk of causing adverse public health effects. In the event of a facility’s registration suspension, it becomes unlawful to distribute, sell, or otherwise introduce or deliver cosmetic products from that facility into the United States. In summary, MoCRA brings forth substantial changes to FDA oversight of the cosmetic industry, mandating registration, listing, safety, and reporting requirements while streamlining FDA enforcement power. Cosmetic manufacturers should prepare for compliance by the December 29, 2023 deadline. _______ Related Services _______ FDA Food Facility Registration Cosmetic Facility Registration & Product Listing (MoCRA) OTC Drug Establishment Registration & Drug Listing Device Establishment Registration & Device Listing _______ Related Services _______ FDA Food Facility Registration Cosmetic Facility Registration & Product Listing (MoCRA) OTC Drug Establishment Registration & Drug Listing Device Establishment Registration & Device Listing
Category: Blog
Your blog category
How to Renew FDA Registration?
How to Renew FDA Registration? How to Renew FDA Registration? FDA Renewal Steps by Step Guide. FDA registration renewal process primarily depends on the type of products that are being marketed in the US. Here we try to break down the FDA renewal steps and fees based on the registration type. In the article below, we cover the FDA renewal steps for food, medical device, drugs and cosmetics. Food Facility Registration Renewal All food facility registrations must be renewed every ‘even year’ between October 1st, and December 31st. Regardless of when a food facility was registered, such registration must be renewed at the end of the following year. For example, if the facility was registered at the end of 2019, it needs to be renewed at the end of 2020 and 2022, 2024, and so on. In short, the steps are: Access FDA registration number and PIN Access FDA FURLS account Review and submit the FDA renewal Receive the FDA renewal notification The FDA food facility registration renewal can be submitted using the FDA FURLS account or via your FDA agent, who has access to the original registration record. Remember, an FDA food facility registration can be transferred between FDA FURLS accounts if the 11-digit FDA registration number and the PIN code are available. It is essential to have to access your FDA number and the PIN code prior to the FDA renewal. The FDA usually sends out a few renewal notices to the registered food facilities during the renewal period, October 1st, and December 31st. If you have questions regarding your FDA FURLS account, you may contact official FDA at [email protected]. The FDA food facility registration is instant, meaning once it is completed, you will receive a renewal confirmation, and you will be all set for another two years. Except for possible FDA US agent fees, there is no fee involved in the FDA food facility renewal. The FDA does not publish the FDA food facility registration data on any public database, and the FDA renewal notification is the only proof you will receive from the FDA. If you need assistance renewing your food facility registration, you may reach us by phone at +1 929-376-7870 or email us at [email protected], and we will assist you. As proof, a certificate of FDA registration will be issued upon completion of the registration renewal. FDA Medical Device Registration Renewal Medical device establishment registration must be renewed annually between October 1st, and December 31st. The FDA Medical device establishment registration renewal involves paying the annual user fee. Once the FDA annual fee is paid, a payment confirmation number PCN will be sent to the applicant, which is needed to renew the medical device establishment. In short, the steps are: Pay the FDA annual device user fee Receive the FDA confirmation PCN Submit the FDA renewal via FURLS Receive the FDA renewal confirmation Keep in mind FDA allows only one FURLS account per device establishment, which means you need to have access to the original FDA account login credentials to be able to renew your device registration. When the device registration is renewed, all associated devices listed under the registration will be automatically renewed, and the records will be published on the FDA device establishment database. The device registration renewal process can be completed within 3-5 days. If you have questions regarding your previous FDA device registration, you may contact official FDA at [email protected]. If you need assistance renewing your device establishment registration, you may contact us by phone at +1 929-376-7870 or email us at [email protected], and we will assist you. As proof, a certificate of FDA registration will be issued upon completion of the registration renewal. Drug Establishment Registration Renewal & Drug Listing Certification FDA Drug establishment registration renewal must be submitted every year between October 1 to December 31. FDA drug registration renewal (or no change notification) can be submitted in SPL format (Structured Product Labeling) via FDA portals, ESG, or CDER Direct. In short, the steps are: Access FDA ESG or CDER account Access the original registration SPL file Submit the renewal/ no change notification Receive the FDA renewal notification Bear in mind the FDA Drug establishment renewal does not involve paying any fees at the time of renewal. However, if you are a manufacturer of a monographed OTC drug, you may be subject to the annual user fee payment under the Over-The-Counter Monograph Drug User Fee Program (OMUFA). The Drug establishment renewal does not automatically mean the drug listings associated with the establishment will also be renewed. The FDA drug listing renewal, known as NDC certification, can be submitted in SPL format via FDA portals, ESG, or CDER Direct. During the certification period, October 1st, through December 31st each year, every active listing on file with the FDA that has not been updated within the current calendar year must be certified that no changes have occurred to remain active for the coming year. If you have questions regarding your FDA CDER account, you may contact the official FDA at [email protected]. Both drug establishment registration and drug listing certification are completed instantly, with no buffer time. Upon completion of drug establishment registration, the record will be updated on the FDA drug establishment database. Likewise, the drug listing certification will be reflected in the FDA NDC directory. If you need assistance renewing your drug establishment registration and drug listings, you can reach us by phone at +1 929-376-7870 or email us at [email protected], and we will assist you. As proof, a certificate of FDA registration will be issued upon completion of the registration renewal. Cosmetic Facility Registration & Cosmetic Product Listing Renewal According to the recently enacted FDA’s Modernization of Cosmetics Regulation Act of 2022 – MoCRA, all registered cosmetic facilities, must promptly update any changes to their registration and renew their registration biennially, every ‘even year’, between October 1, and December 31. Furthermore, all Cosmetic product listings must be updated annually, between October 1 to December 31 via accessing the original registration and listing SPL files. In short, the steps are: Access FDA ESG or CDER account Access the original registration SPL file Submit… Continue reading How to Renew FDA Registration?
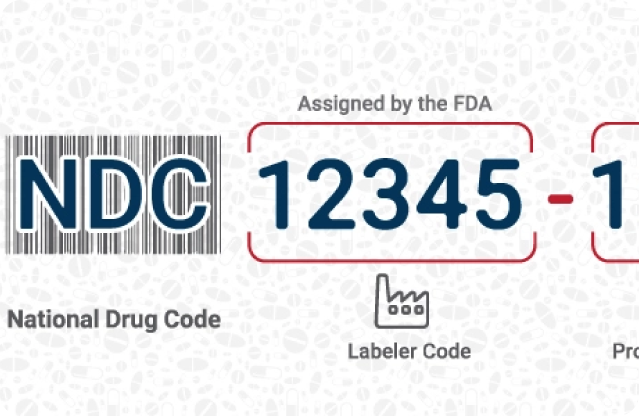
How to obtain NDC number?
How to obtain NDC number? What is NDC number? National Drug Code or NDC is a 10-digit identification number assigned to each drug product in the US market (either OTC or prescription). The NDC number is primarily used for medical billing and insurance purposes, it also can be presented a proof of proper FDA drug listing. The first 5 digits of NDC code, known as labeler code, will be assigned by the FDA to the brand owner, packer and/or the manufacturer of the drug. The second 5 digits will be generated by labeler company according to the drug formulation and the packaging data. How to obtain the Labeler Code? To obtain the Labeler code, the labeler firm must submit a request in SPL format (Structured Product Labeling) via FDA specific portals ESG or CDER Direct. The labeler code request cannot be submitted by email in a paper format. To successfully submit the labeler code application, the applicant must have the firm’s DUNS number and the DUNS record must precisely match the labeler code application data. Below are the steps normally involved in labeler code application process. 1- FDA Labeler code application submission2- Response to possible FDA questions3- Labeler code assignment4- Labeler code activation The labeler code assignment can take up to 10 days. The FDA may contact the applicant for verification purposes. The labeler code application may be rejected by the FDA if the information is not properly submitted or if the applicant cannot provide satisfying answers to FDA questions. If the applicant is a foreign entity, it is mandatory to appoint a US agent for FDA communication purposes. FDA Listing Inc can help your firm with labeler code application and can act as US agent to facilitate the FDA communications. Please contact us by phone +1 929 376 7870 or email us at [email protected] _______ Related Services _______ FDA Food Facility Registration Cosmetic Facility Registration & Product Listing (MoCRA) OTC Drug Establishment Registration & Drug Listing Device Establishment Registration & Device Listing _______ Related Services _______ FDA Food Facility Registration Cosmetic Facility Registration & Product Listing (MoCRA) OTC Drug Establishment Registration & Drug Listing Device Establishment Registration & Device Listing
Medical Devices; Who Must Register List and Pay the Fee
Medical Devices; Who Must Register List and Pay the Fee Establishments that are involved in the production and distribution of medical devices intended for commercial distribution in the U.S., including those that are imported for export only, are required to register annually with the FDA. Most establishments that are required to register are also required to list the devices and the activities performed on those devices at that establishment. The following tabel offers the detail of the requirements for registration and listing based on the type of activity performed at that establishment. The chart also includes a column showing which types of activities require payment of the establishment registration fee. Domestic establishments Foreign establishments Definitions of establishment types Domestic establishments Activity Register List Pay Fee Contract manufacturer(including contract packagers) YES807.20(a)(2) YES807.20(a)(2) YES Contract sterilizer YES807.20(a)(2) YES807.20(a)(2) YES Device being investigated under IDE NO NO807.40(c) NO Domestic Distributor that does not import devices NO807.20(c)(3) NO NO Any establishment located in a foreign trade zone involved with the manufacture, preparation, propagation, compounding, assembly, or processing of a device intended for commercial distribution in the United States YES YES YES Import agent, broker, and other parties who do not take first possession of a device imported into the United States NO NO NO Initial Importer YES807.40(a) NOIdentify manufacturersper 807.20(a)(5) YES Maintains complaint files as required under 21 CFR 820.198 YES YES YES Manufacturer of accessories or components that are packaged or labeled for commercial distribution for health-related purposes to an end user YES807.20(a)(6) YES807.20(a)(6) YES Manufacturer of components, that are not otherwise classified as a finished device, that are distributed only to a finished device manufacturer NO807.65(a) NO NO Manufacturer(including Kit Assemblers) YES807.20(a) YES807.20(a) YES Manufactures a custom device YES807.20(a)(2) YES807.20(a)(2) YES Refurbishers or remarketers of used devices already in commercial distribution in the United States. NO NO NO Relabeler or Repackager YES807.20(a)(3) YES807.20(a)(3) YES Remanufacturer YES YES YES Reprocessor of single use devices YES807.20 YES807.20 YES Specification Consultant Only NO NO NO Specification Developer YES807.20(a)(1) YES807.20(a)(1) YES U.S. Manufacturer of export only devices YES807.20(a)(2) YES807.20(a)(2) YES Wholesale distributor that is not a manufacturer or importer NO NO NO Foreign Establishments Activity Register List Pay Fee Contract Manufacturer(including contract packagers) YES807.40(a) YES807.40(a) YES Contract Sterilizer YES807.40(a) YES807.40(a) YES Custom Device Manufacturers YES807.20(a)(2) YES807.20(a)(2) YES Device Being Investigated under IDE NO812.1 (a) NO812.1(a),807.40(c) NO Foreign Exporter of devices located in a foreign country YES807.40 (a) YES807.40 (a) YES Foreign Manufacturers(including Kit Assemblers) YES807.40(a) YES807.40(a) YES Maintains complaint files as required under 21 CFR 820.198 YES YES YES Manufacturer of accessories or components that are packaged or labeled for commercial distribution for health-related purposes to an end user YES807.20(a)(5) YES807.20(a)(5) YES Manufacturer of components that are distributed only to a finished device manufacturer NO807.65(a) NO NO Relabeler or Repackager YES807.20(a)(3) YES807.20(a)(3) YES Remanufacturer YES YES YES Reprocessor of Single-use Device YES807.20(a) YES807.20(a) YES Specification Developer YES YES YES Definitions of Establishment Activities Contract Manufacturer – Manufactures a finished device to another establishment’s specifications. Contract Sterilizer – Provides a sterilization service for another establishment’s devices. Foreign Exporter – Exports or offers for export to the United States (U.S.), a device manufactured, prepared, propagated, compounded, or processed in a foreign country, including devices originally manufactured in the United States. A foreign exporter must have an establishment address outside the U.S. Initial Importer – Any importer who furthers the marketing of a device from a foreign manufacturer to the person who makes final delivery or sale of the device to the ultimate consumer or user, but does not repackage, or otherwise change the container, wrapper, or labeling of the device or device package. The initial importer must have a physical address in the United States staffed by individuals responsible for ensuring the compliance of imported devices with all applicable FDA laws and regulations. Manufacturer – Makes by chemical, physical, biological, or other procedures, any article that meets the definition of “device” in Section 201(h) of the Federal Food, Drug, and Cosmetic (FD&C) Act. Repackager – Packages finished devices from bulk or repackages devices made by a manufacturer into different containers (excluding shipping containers). Relabeler – Changes the content of the labeling from that supplied from the original manufacturer for distribution under the establishment’s own name. A relabeler does not include establishments that do not change the original labeling but merely add their own name. Remanufacturer – Any person who processes, conditions, renovates, repackages, restores, or does any other act to a finished device that significantly changes the finished device’s performance or safety specifications, or intended use. Reprocessor of Single Use Device – Performs remanufacturing operations on a single use device. Specification Developer – Develops specifications for a device that is distributed under the establishment’s own name but performs no manufacturing. This includes establishments that, in addition to developing specifications, also arrange for the manufacturing of devices labeled with another establishment’s name by a contract manufacturer. U. S. manufacturer of export only devices – Manufactures medical devices that are not sold in the U.S. and are manufactured solely for export to foreign countries. Source: www.fda.gov _______ Related Services _______ FDA Food Facility Registration Cosmetic Facility Registration & Product Listing (MoCRA) OTC Drug Establishment Registration & Drug Listing Device Establishment Registration & Device Listing _______ Related Services _______ FDA Food Facility Registration Cosmetic Facility Registration & Product Listing (MoCRA) OTC Drug Establishment Registration & Drug Listing Device Establishment Registration & Device Listing
FDA Requirements for Hand Sanitizers and Other Antiseptic OTC Drugs
FDA Requirements for Hand Sanitizers and Other Antiseptic OTC Drugs Hand Sanitizers and most form of antiseptic/antibacterial products are considered over-the-counter (OTC) drugs by the FDA. In order to introduce an OTC drug to the U.S. market, the manufacturers must fulfill certain FDA requirements that are summarized below. OTC Drug Manufacturers: Follow the relevant OTC monograph published by the FDA in compounding/formulation of the hand sanitizer (as well as GMP). Register the Drug Manufacturing Establishment with the FDA and assign a US agent (official correspondent) Obtain the National Drug Code , NDC List the Drug with the FDA and submit the final label of the drug product Comply with the FDA Drug Labeling Requirements U.S. OTC Drug Importer / Private Label Distributor: Obtain the National Drug Code , NDC List the Drug with the FDA and submit the final label of the drug product Comply with the FDA Drug Labeling Requirements The registration and listing process can take 6-8 workdays depending on how quickly you can provide the FDA-required information. Note, FDA may not need to conduct site inspection prior to allowing you to sell in the US market, however the FDA can inspect manufacturing plant at any point to verify the GMP (Good Manufacturing Practice) compliance. FDA’s Temporary Policies for Alcohol-Based Hand Sanitizers in response to COVID-19 In the light of the current dynamic due to the COVID-19 pandemic the FDA has recently published two guidance documents for industry for compounding pharmacies as well as companies not typically regulated by the FDA . What are key points in FDA new policy? The hand sanitizer should be made according to specific formulations and by using U.S. Pharmacopoeia-grade ingredients listed below: o Isopropyl Alcohol (75%, volume/volume) or Alcohol (ethanol 80% volume/volume) in a water containing solution o Glycerol (1.45% volume/volume) o Hydrogen peroxide (0.125% volume/volume) o Sterile distilled water / boiled and cooled water Manufacturer should utilize the most accurate method for analyzing the alcohol content of each batch of finished product. The sanitizer products must be prepared under sanitary conditions that have appropriate equipment’s in place. OTC Drug products that do meet such FDA conditions must follow the FDA’s standard drug requirements for approval (OTC monograph, new drug application-NDA, etc.). FDA Listing Inc. is helping companies with the U.S. FDA compliance. If you are planning to market hand sanitizers or any form of antiseptic products, we can help you in fulfilling FDA requirements. Feel free to call us at +1 929-376-7870 or chat with our regulatory advisors for immediate assistance. _______ Related Services _______ FDA Food Facility Registration Cosmetic Facility Registration & Product Listing (MoCRA) OTC Drug Establishment Registration & Drug Listing Device Establishment Registration & Device Listing _______ Related Services _______ FDA Food Facility Registration Cosmetic Facility Registration & Product Listing (MoCRA) OTC Drug Establishment Registration & Drug Listing Device Establishment Registration & Device Listing
How Exactly Cosmetics Are Not FDA Approved, but They Are FDA Regulated
How Exactly Cosmetics Are Not FDA Approved, but They Are FDA Regulated The law does not require cosmetic products and ingredients, other than color additives, to have FDA approval before they go on the market in the U.S., but there are FDA laws and regulations that apply to cosmetics on the market in the U.S. commerce. The two most important laws relating to cosmetics marketed in the United States are the Federal Food, Drug, and Cosmetic Act (FD&C Act) and the Fair Packaging and Labeling Act (FPLA). In the United States, federal laws are enacted by Congress. In order to make the laws work on a day-to-day level, Congress authorizes certain government agencies. such as FDA, to create regulations. A change in FDA’s legal authority over cosmetics would require Congress to change the law. What kinds of products are “cosmetics” under the law? The FD&C Act defines cosmetics by their intended use, as “articles intended to be rubbed, poured, sprinkled, or sprayed on, introduced into, or otherwise applied to the human body…for cleansing, beautifying, promoting attractiveness, or altering the appearance” Among the products included in this definition are skin moisturizers, perfumes, lipsticks, fingernail polishes, eye and facial makeup, cleansing shampoos, permanent waves, hair colors, and deodorants, as well as any substance intended for use as a component of a cosmetic product. It does not include soap. But, if the product is intended for a therapeutic use, such as treating or preventing disease, or to affect the structure or function of the body, it’s a drug (FD&C Act, 201(g)), or in some cases a medical device (FD&C Act, 201(h)), even if it affects the appearance. Other “personal care products” may be regulated as dietary supplements or as consumer products. The information presented here applies only to the regulation of products that are cosmetics as defined by the FD&C Act. What does the law say about the safety and labeling of cosmetics? The FD&C Act prohibits the marketing of adulterated or misbranded cosmetics in interstate commerce. “Adulteration” refers to violations involving product composition–whether they result from ingredients, contaminants, processing, packaging, or shipping and handling. Under the FD&C Act, a cosmetic is adulterated if– “it bears or contains any poisonous or deleterious substance which may render it injurious to users under the conditions of use prescribed in the labeling thereof, or under conditions of use as are customary and usual” (with an exception made for coal-tar hair dyes); “it consists in whole or in part of any filthy, putrid, or decomposed substance”; “it has been prepared, packed, or held under insanitary conditions whereby it may have become contaminated with filth, or whereby it may have been rendered injurious to health”; “its container is composed, in whole or in part, of any poisonous or deleterious substance which may render the contents injurious to health”; or except for coal-tar hair dyes, “it is, or it bears or contains, a color additive which is unsafe within the meaning of section 721(a)” of the FD&C Act. (FD&C Act, sec. 601) “Misbranding” refers to violations involving improperly labeled or deceptively packaged products. Under the FD&C Act, a cosmetic is misbranded if– “its labeling is false or misleading in any particular”; its label does not include all required information. (An exemption may apply to cosmetics that are to be processed, labeled, or repacked at an establishment other than where they were originally processed or packed. the required information is not adequately prominent and conspicuous; “its container is so made, formed, or filled as to be misleading”; it is a color additive, other than a hair dye, that does not conform to applicable regulations issued under section 721 of the FD&C Act; and “its packaging or labeling is in violation of an applicable regulation issued pursuant to section 3 or 4 of the Poison Prevention Packaging Act of 1970.” (FD&C Act, sec. 602) Under the FD&C Act, a product also may be misbranded due to failure to provide material facts. This means, for example, any directions for safe use and warning statements needed to ensure a product’s safe use. In addition, under the authority of the FPLA, FDA requires a list of ingredients for cosmetics marketed on a retail basis to consumers (Title 21, Code of Federal Regulations (CFR), section 701.3). Cosmetics that fail to comply with the FPLA are considered misbranded under the FD&C Act. (FPLA, section 1456) This requirement does not apply to cosmetics distributed solely for professional use, institutional use (such as in schools or the workplace), or as free samples or hotel amenities. FDA can take action against cosmetics on the market that are in violation of these laws, as well as companies and individuals who market such products. Does FDA approve cosmetics before they go on the market? FDA’s legal authority over cosmetics is different from our authority over other products we regulate, such as drugs, biologics, and medical devices. Under the law, cosmetic products and ingredients do not need FDA premarket approval, with the exception of color additives. However, FDA can pursue enforcement action against products on the market that are not in compliance with the law, or against firms or individuals who violate the law. In general, except for color additives and those ingredients that are prohibited or restricted by regulation, a manufacturer may use any ingredient in the formulation of a cosmetic, provided that– the ingredient and the finished cosmetic are safe under labeled or customary conditions of use, the product is properly labeled, and the use of the ingredient does not otherwise cause the cosmetic to be adulterated or misbranded under the laws that FDA enforces. Who is responsible for substantiating the safety of cosmetics? Companies and individuals who manufacture or market cosmetics have a legal responsibility to ensure the safety of their products. Neither the law nor FDA regulations require specific tests to demonstrate the safety of individual products or ingredients. The law also does not require cosmetic companies to share their safety information with FDA. FDA has consistently advised manufacturers to use whatever testing… Continue reading How Exactly Cosmetics Are Not FDA Approved, but They Are FDA Regulated
N95 Respirators and Surgical Masks (Face Masks)
N95 Respirators and Surgical Masks (Face Masks) N95 respirators and surgical masks (face masks) are examples of personal protective equipment that are used to protect the wearer from airborne particles and from liquid contaminating the face. Centers for Disease Control and Prevention (CDC) National Institute for Occupational Safety and Health (NIOSH) and Occupational Safety and Health Administration (OSHA) also regulate N95 respirators. It is important to recognize that the optimal way to prevent airborne transmission is to use a combination of interventions from across the hierarchy of controls, not just PPE alone. N95 Respirators Not for Use by the Public The Centers for Disease Control and Prevention (CDC) does not recommend that the general public wear N95 respirators to protect themselves from respiratory diseases, including coronavirus (COVID-19). The best way to prevent illness is to avoid being exposed to this virus. However, as a reminder, CDC always recommends everyday preventive actions, such as hand washing, to help prevent the spread of respiratory diseases. For the general American public, there is no added health benefit to wear a respiratory protective device (such as an N95 respirator), and the immediate health risk from COVID-19 is considered low. Surgical Masks (Face Masks) The Centers for Disease Control and Prevention (CDC) does not recommend that people who are well wear a face mask to protect themselves from respiratory diseases, including coronavirus (COVID-19). A surgical mask is a loose-fitting, disposable device that creates a physical barrier between the mouth and nose of the wearer and potential contaminants in the immediate environment. Surgical masks are regulated under 21 CFR 878.4040. Surgical masks are not to be shared and may be labeled as surgical, isolation, dental, or medical procedure masks. They may come with or without a face shield. These are often referred to as face masks, although not all face masks are regulated as surgical masks. Surgical masks are made in different thicknesses and with different ability to protect you from contact with liquids. These properties may also affect how easily you can breathe through the face mask and how well the surgical mask protects you. If worn properly, a surgical mask is meant to help block large-particle droplets, splashes, sprays, or splatter that may contain germs (viruses and bacteria), keeping it from reaching your mouth and nose. Surgical masks may also help reduce exposure of your saliva and respiratory secretions to others. While a surgical mask may be effective in blocking splashes and large-particle droplets, a face mask, by design, does not filter or block very small particles in the air that may be transmitted by coughs, sneezes, or certain medical procedures. Surgical masks also do not provide complete protection from germs and other contaminants because of the loose fit between the surface of the face mask and your face. Surgical masks are not intended to be used more than once. If your mask is damaged or soiled, or if breathing through the mask becomes difficult, you should remove the face mask, discard it safely, and replace it with a new one. To safely discard your mask, place it in a plastic bag and put it in the trash. Wash your hands after handling the used mask. N95 Respirators An N95 respirator is a respiratory protective device designed to achieve a very close facial fit and very efficient filtration of airborne particles. The ‘N95’ designation means that when subjected to careful testing, the respirator blocks at least 95 percent of very small (0.3 micron) test particles. If properly fitted, the filtration capabilities of N95 respirators exceed those of face masks. However, even a properly fitted N95 respirator does not eliminate the risk of illness or death. Comparing Surgical Masks and Surgical N95 Respirators The FDA regulates surgical masks and surgical N95 respirators differently based on their intended use. A surgical mask is a loose-fitting, disposable device that creates a physical barrier between the mouth and nose of the wearer and potential contaminants in the immediate environment. These are often referred to as face masks, although not all face masks are regulated as surgical masks. Note that the edges of the mask are not designed to form a seal around the nose and mouth. An N95 respirator is a respiratory protective device designed to achieve a very close facial fit and very efficient filtration of airborne particles. Note that the edges of the respirator are designed to form a seal around the nose and mouth. Surgical N95 Respirators are commonly used in healthcare settings and are a subset of N95 Filtering Facepiece Respirators (FFRs), often referred to as N95s. The similarities among surgical masks and surgical N95s are: They are tested for fluid resistance, filtration efficiency (particulate filtration efficiency and bacterial filtration efficiency), flammability and biocompatibility. They should not be shared or reused. General N95 Respirator Precautions People with chronic respiratory, cardiac, or other medical conditions that make breathing difficult should check with their health care provider before using an N95 respirator because the N95 respirator can make it more difficult for the wearer to breathe. Some models have exhalation valves that can make breathing out easier and help reduce heat build-up. Note that N95 respirators with exhalation valves should not be used when sterile conditions are needed. All FDA-cleared N95 respirators are labeled as “single-use,” disposable devices. If your respirator is damaged or soiled, or if breathing becomes difficult, you should remove the respirator, discard it properly, and replace it with a new one. To safely discard your N95 respirator, place it in a plastic bag and put it in the trash. Wash your hands after handling the used respirator. N95 respirators are not designed for children or people with facial hair. Because a proper fit cannot be achieved on children and people with facial hair, the N95 respirator may not provide full protection. N95 Respirators in Industrial and Health Care Settings Most N95 respirators are manufactured for use in construction and other industrial type jobs that expose workers… Continue reading N95 Respirators and Surgical Masks (Face Masks)
What Do The Importers Need to Know About The FDA’s FSVP
What Do The Importers Need to Know About The FDA’s FSVP Conversation with Sharon Mayl The first major compliance date for importers covered by the Foreign Supplier Verification Programs (FSVP) rule arrives on May 30, 2017. FSVP is mandated by the FDA Food Safety Modernization Act (FSMA). FSVP requires importers to verify that their foreign suppliers of food for human and animal consumption meet applicable FDA safety standards. More specifically, FSVP requires importers to verify that their suppliers are producing food using procedures that offer same level of public health protection as the preventive controls (PC) requirements in the preventive controls and current good manufacturing practices rules for human and animal food and produce safety FSMA rules, and that the food is properly labeled with respect to allergens. Sharon Mayl, Senior Advisor for Policy in the Office of Foods and Veterinary Medicine at FDA, explains what importers need to know when facing this May compliance date and what lies ahead for FSVP implementation. Q: When are the compliance dates for the FSVP rule? It is important to note the compliance dates for FSVP are not based on the size of the importer. Instead, the compliance dates are staggered based on the size of the foreign supplier and the regulations that apply to the foreign supplier. The first compliance date is eighteen months after the FSVP final rule was published in the Federal Register. This date gives importers sufficient time to understand the rule and develop their FSVPs. After that, importers generally have to comply six months after their foreign supplier has to be in compliance with the PC or produce safety rules. We linked the FSVP compliance dates to the other FSMA rules because we wanted to minimize the likelihood that an importer would be required to comply with the FSVP regulation before its supplier is required to comply with other FSMA food safety regulations. Q: Who must be in compliance with the FSVP requirements by May 30, 2017? U.S. importers subject to this first compliance date have foreign suppliers that fall into one of three categories: Foreign suppliers that will not be covered by the PC or produce safety rules; Foreign suppliers subject to the PC for Human Food rule and are not “small businesses,” “qualified facilities” (certain very small businesses) or subject to the Pasteurized Milk Ordinance; or Foreign suppliers subject to the current good manufacturing practices (CGMP) requirements in the PC for Animal Food rule, and are not “small businesses” or “qualified facilities”. For ease of viewing, we have a chart on fda.gov titled “Am I Subject to FSVP?” that importers can refer to if they are unsure if the rule applies to them. Q: What do importers have to verify on May 30, 2017? Importers covered by the FSVP rule will have to verify that their suppliers meet applicable FDA food safety requirements, including that the food is not adulterated or misbranded with respect to allergens. The largest foreign suppliers subject to the PC for Human Food rule had to be in compliance in September 2016 with both the PC provisions and the CGMP requirements of that rule, but the largest suppliers subject to the PC for Animal Food rule only had to be in compliance with the CGMP requirements by that date. Therefore, importers of foods from those facilities will only need to consider those provisions of the PC rules that their suppliers have had to come in compliance with by May 30, as well as verify that the food is not adulterated or misbranded with respect to allergens. And I want to clarify that importers have some flexibility with respect to the PC and produce safety rules. Importers will need to have a program that allows them to demonstrate that their foreign suppliers are producing food in a manner that provides the same level of public health protection as the PC or produce rules. As noted above, importers will have additional time to develop and implement FSVPs for foods from smaller suppliers that are considered qualified facilities or small businesses under the PC rules, as well for food subject to the produce safety rule. Q: When the first compliance dates arrived in September 2016 for the preventive controls rules, FDA indicated that it would focus on education, training, and technical assistance. Is that also true for this FSVP compliance date? Yes, we have done a lot of outreach already to help importers understand the regulations and what they have to do. However, we understand that this is new to a lot of importers, so our approach will be to educate while we regulate to create a culture of compliance. Importers can expect interactive FDA inspections with opportunities to explain how their programs meet our requirements and how they will take corrective actions if we observe deficiencies. Good communication is key. Our initial enforcement priorities will be, as they are now, on food safety problems that pose an imminent public health risk. But the FDA’s mandate is to protect public health and, when appropriate, the agency will act swiftly. Q: Will FSVP change the admission process? All foods regulated by the FDA will see changes to the entry process as of May 30, 2017. When food is offered for entry into the United States, the Customs and Border Patrol (CBP) Automated Commercial Environment (ACE) system will require the filer to enter at least one additional code as part of the required data elements. An FSVP importer subject to the May 30 compliance date should use the entity role code “FSV,” indicating the entry is subject to the FSVP regulation. This will then prompt the ACE system to ask for the importer’s name, email address, and unique facility identifier (UFI) recognized as acceptable by FDA. We recently issued guidance formally recognizing the Data Universal Numbering System (DUNS) number as an acceptable UFI for FSVP. Conversely, if the food entry line is exempt from the requirements of FSVP, or not yet subject to the rule because it has a later compliance date, the filer should… Continue reading What Do The Importers Need to Know About The FDA’s FSVP